The Problem:
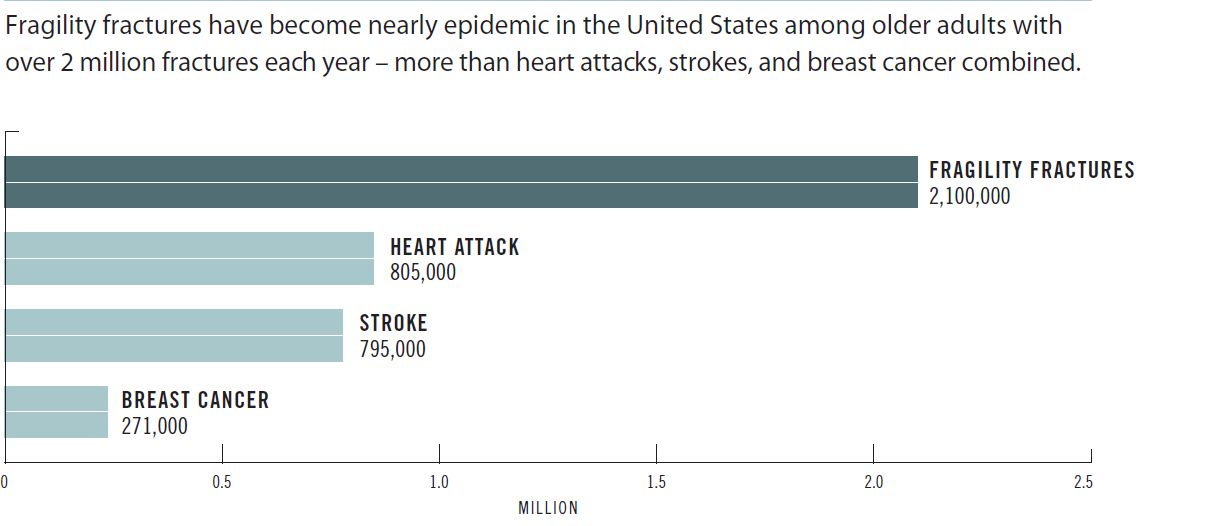
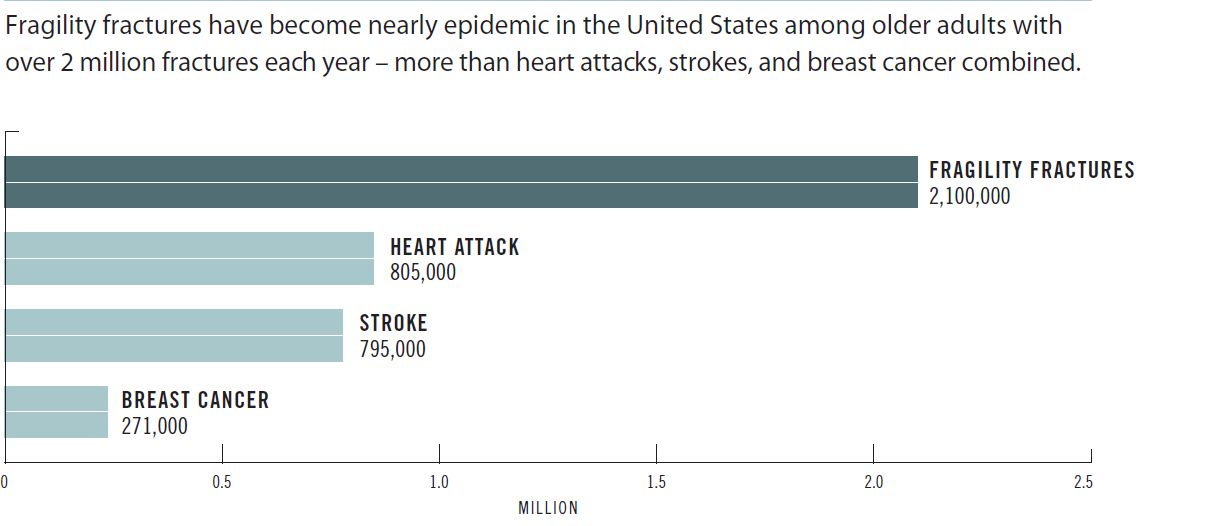
Less than half of these patients will not receive the recommended osteoporosis care following their fractures. A fragility fracture is a key predictor of future fractures.
The Solution:
Help close the osteoporosis treatment gap by establishing a systems-based approach at your institution. Own the Bone is a quality improvement program to address the osteoporosis treatment gap and prevent subsequent fragility fractures. Own the Bone provides a simple, easy-to-use tool to enable hospitals, medical centers, and practices to establish a bone health program or fracture liaison service (FLS) to:
- Identify, evaluate and treat fragility fracture patients over 50 at risk of osteoporosis.
- Coordinate patient care among different specialties and physicians for each patient.
Through a clinically-proven, web-based patient registry and 10 prevention measures, Own the Bone seeks to:
- Close the post-fracture treatment gap documented in the RAND and NCQA studies as it applies to physician treatment recommendations
- Change physician and patient behavior to reduce the incidence of future fractures and impact of osteoporosis
- The program focuses on osteoporosis diagnosis and cares following a fracture, rather than primary osteoporosis prevention.
FLS Programs Target Patients Likely to Have Subsequent Fractures
Fragility fractures are an independent predictor of future fractures. Patients who have had prior fractures are at a higher risk for future fractures. In particular, perimenopausal and postmenopausal women with a prior fracture have twice the risk of subsequent fracture.